Retina & Vitreous
The Vitreoretinal Service at Saraswati Nethralaya offers expertise in diagnostic, medical and surgical retina. Diagnostics forming the backbone of every successful treatment, we provide a very advanced small pupil fundus camera for Fundus Fluorescein Angiography, and a precise Optical Coherence Tomography system. Treatment of all retinopathies affecting the eye due to diabetes, hypertension, vascular malformations and age related macular degeneration is possible with laser and anti-VEGF injections or surgery depending on the requirement. The retina laser service houses an advanced Argon-Laser System for Retinal Photocoagulation and also the Photo Dynamic Therapy laser system for treatment of Age Related Macular Degeneration. For Surgical treatment the department is equipped with advanced Micro Incision Vitreous surgery system and with its team of expert surgeons caters to advanced retina surgery requirements including Retina Detachments, Ocular Trauma, Diabetic Micro Incision Vitreous surgery, Macular Hole surgery etc.
The Retina
The Retina is an extremely crucial structure for vision. It is located in the posterior segment (back of our eye). In lay terms it is called the curtain of the eye.
The retina can be divided into two regions: the central (macula) and the peripheral. The macula is a very small area in the centre of the retina upon which light rays are focused by the cornea and the lens of the eye. The macula being the most sensitive portion of the retina is responsible for acute (sharp) vision, that is for reading, writing, threading a needle and other fine tasks. The periphery of the retina gives us vision to the side, which is called peripheral vision. This is what we refer to when we say, I saw something from the corner of my eye.
Common Retinal Disoders include-
DIABETIC RETINOPATHY
AGE RELATED MACULAR DEGENERATION
VASCULAR OCCLUSIONS
RETINAL DETACHMENT
Imaging Modalities
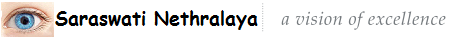
Fluorescein Angiography (FA)
A special dye (Sodium Fluorescein) is injected into your vein and serial photographs of the retina are taken. The photographs may reveal leaking new vessels (choroidal neovascular membrane), define its location in reference to the centre point and determine any associated finding i.e. hemorrhage, exudates. Fluorescein angiography is an important tool in planning treatment and a recent angiogram is essential at the time of treatment. Repeat angiograms after treatment are indicated to confirm the status of the lesion.
Indocyanine Green Angiography (ICGA)
ICGA gives a better study of the deeper (choroidal) circulation. It is indicated in certain cases where the fluorescein angiography is inconclusive e.g. cases with ill-defined membranes, presence of hemorrhage, or polypoidal vasculopathy. It takes longer than fluorescein angiography as photographs are taken till 20 minutes after injection of dye.

Optical Coherence Tomography (OCT)
This is a newer noninvasive test, which gives an accurate structural analysis of the retina. It is a non contact scan which provides very high resolution imaging without the need for any injection of any dye etc. At Saraswati Nethralaya we have acquired the latest SPECTRAL DOMAIN OCT machines which have a resolution of 5 microns! It is helpful in diagnosis and very importantly in follow-up of the disease.
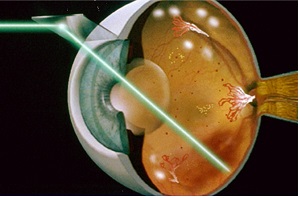
Laser Photocoagulation
Laser for long has been the mainstay of treatment for many retina disorders as Diabetic Retinopathy, Vascular Occlusion, Age Related Macular Degeneration, Vascular Malformations and as a prophylaxis treatment for Retina Tears and Lattice Degenerations. Photo Dynamic Therapy a newer modality for treatment of age related macular degeneration and is very useful for specific indications. It is a safe modality in cases where therapy is needed close to the fine vision area of the retina. Laser is often a preventive modality that enables our patients to preserve their vison, enabling them to see a better tomorrow.

Intravitreal Injections
Oedema or swelling at the macula (The central fine vision area of the retina) known as Macular Oedema can be well treated with Anti-VEGF injections of Lucentis, Avastin and Triamcinolone Acetate. For years our patients have and are being treated with these injections at regular intervals with improvement in vision and decrease in oedema. AntiVEGF injections also play a very important role in the treatment of wet AMD and have been used at our centre for years with appreciable and significant treatment results .
OZURDEX
A novel intravitreal drug delivery system has been developed that gradually releases the steroid dexamethasone after it has been inserted into the eye through a small puncture. It is composed of biodegradable copolymers. As dexamethasone is released, the polymer slowly degrades into carbon dioxide and water. Since the implant eventually dissolves completely, sequential implants can be placed into the eye over time without the need for surgical removal. It has shown great benefit in treatment of macular oedema due to retinal vein occlusions.
Surgical Treatment Modalities
Scleral Buckle
A traditional procedure for treatment of Retinal Detachment assures long term anatomical attachment of the retina. With its benefits and the special expertise of our surgeons at the procedure, a very high number of our patients have benefitted over the years and still is one of the most promising procedure of treatment of Retinal Detachment especially in the younger age group.
Vitreo-Retinal Surgery
Vitrectomy is now a routinely performed surgery for several retinal disorders,. Recently we are performing these surgeries with much finer and more precise instrumentation. This is known as Micro-Incision Vitreous Surgery (MIVS). It has resulted more precise, technically advanced and safe surgery with better outcomes for the patient along with a faster recovery. Micro-Incision Vitreous Surgery remains the mainstay for surgical treatment of various disorders of the Vitreo-retina specially in use for Diabetic Retinopathy, Retinal Detachment , vitreous haemorrhage ,Macular Holes and ERM , endophthalmitis etc .
Diabetic Retinopathy
DIABETES MELLITUS is a condition that impairs the body's ability to use and store sugar (glucose). Sugar is excreted in the urine and the blood sugar is abnormally high. It causes changes in small blood vessels in various organs of the body. Diabetes can cause various changes in the eye as well, particularly in the retina. Diabetic eye disease can cause severe vision loss or even blindness. At Saraswati Nethralaya, we have a dedicated team of Vitreo-Retinal specialists committed to provide you with the best possible care to protect your vision.
What is Diabetic retinopathy?
When the retina is affected by diabetes, weakened blood vessels may leak fluid or blood, causing damage to the retina. This is called DIABETIC RETINOPATHY.
There are two forms of diabetic retinopathy. In BACKGROUND RETINOPATHY, blood vessels within the retina become abnormally permeable and allow substances like fluid and lipid to leak out. This results in water logging or edema of retinal tissue and deposition of yellowish material called exudates. If the leaking fluid collects in the macula (the central part of the retina responsible for reading vision and other fine tasks), vision gets affected, often to a marked degree.
The second form is PROLIFERATIVE RETINOPATHY. Abnormal fragile new blood vessels grow on the surface of the retina or optic nerve and sometimes into the vitreous cavity. These fragile vessels may rupture and bleed into the normally clear vitreous gel, blocking light from reaching the retina. Subsequent scar formation in the vitreous may pull on the retina, detaching it from the back of the eye (traction retinal detachment). Severe loss of sight, blindness, and even painful glaucoma can result from these conditions.
What are the Symptoms?
Please note that every person with diabetes need not have Diabetic Retinopathy. Conversely an eye with marked changes of Diabetic Retinopathy can have good vision and be totally free of symptoms. Hence it is important for all diabetics to undergo REGULAR EYE CHECK-UP INCLUDING RETINAL EXAMINATION THROUGH DILATED PUPILS especially for people who have been diabetic for a number of years. It is also true that diabetes is often detected in a person, when some changes of retinopathy are seen on routine examination of the eye.
Reduced central vision can occur if the macula gets edematous (swollen). Black spots (floaters) and cobwebs of sudden onset often point to a minor bleed inside the eye. Sudden total loss of vision may occur due to a large bleed into the vitreous.
Investigations for Diabetic Retinopathy
If diabetic retinopathy is noted, color photographs of the retina may be taken and FLUORESCEIN ANGIOGRAPHY performed. This involves dilating the pupils and injection of a fluorescent dye into a vein in the arm. Photographs of the retina are taken rapidly as the dye passes through the retinal blood vessels. This test helps in determining if laser photocoagulation treatment is necessary. If treatment is to be done, it helps in identifying what structures and areas need treatment with laser.
OPTICAL COHERENCE TOMOGRAPHY (OCT), which is newer non-invasive diagnostic modality provides a cross-sectional view of the retina and helps in quantifying the amount and type of swelling and guides the treatment.
Treatment of Diabetic Retinopathy
PHOTOCOAGULATION involves the use of a LASER beam to seal leaking blood vessels and prevent growth of abnormal blood vessels. This procedure does not require hospitalization. In background retinopathy, if blood vessels are leaking fluid into the macula, laser treatment stops the leakage and may improve or stabilize vision. In proliferative retinopathy, laser treatment may involve one or more sessions depending on the type and severity of retinopathy. Laser treatment significantly reduces the chances of severe visual loss by destroying the abnormal blood vessels and preventing growth of more such vessels. Vision may improve or stabilize within several weeks to a year. It is important to remember that laser treatment is not a one-time procedure. Regular follow up is extremely important. Your doctor will tell you when to return for a check-up.
Recently, along with laser treatment, certain medication when injected into the eye or just outside the eye has shown encouraging results. These medicines include intravitreal Avastin, lucentis as well as steroids. They often need to be repeated in order to keep the swelling in check. Being injected into the eye they are however to be used cautiously and judiciously.
If the vitreous is too clouded with blood or there is traction retinal detachment, laser treatment will not work. In this situation, a surgical procedure called VITRECTOMY needs to be performed. In this operation, opaque vitreous gel is removed from within the eye by a special instrument that simultaneously sucks and cuts the vitreous.
Prevention of Diabetic Retinopathy
LOSS OF VISION FROM DIABETIC RETINOPATHY IS LARGELY PREVENTABLE.
EARLY DETECTION of diabetic retinopathy is the best protection against sight loss. This is possible by having a complete eye examination including retina check-up once a year or more frequently if advised. In most cases the ophthalmologist can then begin treatment before sight is affected.
Excellent control of diabetes and associated conditions like hypertension, increased blood lipids & cholesterol and renal (kidney) disease, is strongly recommended. However, good control in itself does not guarantee freedom from diabetic retinopathy.
Age Related Macular Degeneration
Globally, Age Related Macular Degeneration (AMD) is the third most common cause of legal blindness (WHO 2002) whilst in most western countries it is by far the commonest cause of blindness. Macular degeneration usually manifests after 50 years of age. With the rapid rise in the geriatric age group, which is the at risk group, the disorder could take epidemic proportions and become a major public health consideration. At Saraswati Nethralaya, we have a dedicated team of Vitreo-Retinal specialists committed to provide you with the best possible care to protect your vision.
Definition of Age Related Macular Degeneration
Age Related Macular Degeneration (AMD) is a disease associated with aging, characterized by damage to the central part of the retina called macula. Before we talk about what can go wrong, it is important to understand how the eye works when it is working properly.
Dry AMD
It is the most common form found in 90% of patients. Dry AMD occurs when the macular tissues get thin and slowly lose function. The most common symptom of dry AMD is blurred vision which causes difficulty in recognizing faces, increases light requirement for reading and other tasks. Visual deterioration is slow but usually not profound. About 10-20% of people with dry AMD advance to the wet form.
Wet AMD
It is the less common but more aggressive form of AMD. If it is not treated it may get worse rapidly. Wet AMD is caused by proliferation of abnormal blood vessels under the retina which may exude or leak out fluid, or bleed and ultimately lead to the formation of a scar under the retina. The various treatment options to stall progress to the wet form and to restrict vision loss will be discussed.
Symptoms of AMD
- Diminution of vision in an important symptom of macular degeneration. This lack of ability to see objects clearly affects ones ability to read, drive and see details.
- Straight lines appear crooked or wavy.
- A dark area appears in the centre of vision e.g. words in the central part of the page look smudged.
Having one or more of these symptoms may not necessarily mean that one has AMD and it warrants an immediate eye check up (early detection is important).
Risk Factors for AMD
Age is the greatest risk factor. Although AMD can occur during middle age, studies show that people over 60 years of age are at great risk. The risk increases with increasing age.
Family History of AMD increases the risk.
Race White populations are more predisposed to suffer vision loss from neovascular AMD than Asian or African populations.
Smoking has a definite correlation
History of hypertension, heart disease, or lung infection adds to risk.
Detection of AMD
Early detection is of paramount importance as smaller lesions have a better recovery and chance of maintaining reading vision than advanced cases with larger lesions and fibrotic changes.
Your ophthalmologist may suspect AMD if you are over 60 years of age and have recent changes in central vision. To establish a diagnosis a comprehensive eye check up is done.
Visual Acuity test This eye chart test measures how well you see at varying distances.
Amsler Grid In this test the patient wearing his reading glasses, covers the opposite eye and looks at the black dot in the centre of the test page (checker board pattern) to check for any area which is distorted, blurred, discolored or not visible. It is a useful test to detect early changes and can be done routinely by the patient at home.
Dilated eye examination To look for signs of the disease your doctor will use drops to dilate or widen the pupil. With a special magnifying lens and a light source your doctor will examine your retina. Dilating drops hamper close vision for around 4-5 hours.
If on the above examination your doctor suspects AMD, other tests to learn more about the structure and functioning of the retina could be advised.
Treatment Of Wet Age-Related Macular Degeneration
Wet AMD can be treated with laser photocoagulation, photodynamic therapy, intravitreal injections or a combination of these. The aim of treatment is to slow the rate of vision decrease or stop further vision loss but the disease some times may progress despite treatment. With the advent of anti-VEGF treatment there are greater numbers of patients who are showing visual improvement.
Laser photocoagulation
This out patient procedure uses the conventional laser to destroy fragile, leaking blood vessels. A high energy beam of light aimed directly on the new blood vessels, destroys and inactivates them, preventing further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue. Only a small percentage of patients where the membrane is away from the centre (fovea) can be treated by this modality. Re-treatments may be necessary. Recently in some cases we combine it with an anti-VEGF agent so as to decrease the chances of recurrence.
Photodynamic Therapy (PDT)
Photodynamic therapy (PDT) has been found to be an effective treatment for patient for patients with new vessels (choroidal neovascular membrane or CNVM) secondary to AMD, myopia, etc. It reduces the risk of moderate and severe vision loss. A light stimulated drug called Verteporfin is injected intravenously. It travels through out the body including the new vessels in the eye. The drug tends to stickR to the surface of new blood vessels. Next a low intensity laser beam (689nm) is directed into the eye for about 83 seconds to activate the drug. The activated drug selectively destroys the abnormal blood vessels without damage to surrounding healthy tissue. Because the drug is activated by light the patient must avoid exposure of skin or eyes to direct sunlight or bright indoor light for 5 days after treatment. The treatment is relatively painless and no major side effects have been reported. PDT slows the rate of vision loss. Re-treatment may be required but usually not before 3 months.
Intravitreal Injections (Anti-VEGF Agents)
Abnormally high levels of Vascular Endothelial Growth Factor (VEGF) occur in eyes with wet AMD which promotes the growth of abnormal new blood vessels. Anti-VEGF agents block the effects of this growth factor. Treatment by this agent helps slow down vision loss from AMD and in some case improves vision. Multiple injections are often required for complete inactivation of the disease process.
Avastin (Bevacizumab) is an anti-VEGF agent approved for use in colorectal cancer. Ophthalmologists are using it's off label in AMD and other vascular conditions for its anti-angiogenic property. When used in the eye as an intravitreal injection its dose is miniscule and risk of adverse systemic reactions like gastrointestinal perforation, thrombo-embolic reactions, hypertension and proteinuria is negligible. There are no formal clinical trials with Avastin but recent experience with this drug has been encouraging with most patients getting stabilized and some improving.
Macugen (Pegaptanib Sodium) is the first selective VEGF inhibitor which the FDA approved to treat the pathologic process underlying all subtypes of neovascular AMD. In clinical studies Macugen was given every 6 weeks for upto two years and was found to preserve visual acuity of all subtypes of neovascular AMD. Its advantage lies in its selective systemic inhibition of VEGF, thereby making it possible for use in patients with recent cardiac history.
Lucentis (Ranibizumab) is a recently FDA approved anti-VEGF agent that neutralizes all active forms of vascular endothelial growth factor. It is a recombinant homogenized monoclonal antibody. Clinical trials with Lucentis have shown not only stabilization but also improvement in visual acuity. In the multicentre trial comparing effectivity of Lucentis to sham injection for minimally classic or occult CNVM, it was found that 94.5% of the group given 0.3 mg and 94.6 % of those given 0.5mg had stable vision compared with 62.2 % of those receiving the sham injection. Visual acuity improved in 24.8 % of the 0.3 mg group and 33.8% of 0.5 mg group as compared with 5% of the sham injection group. The benefit in visual acuity was maintained at 24 months. Lucentis was also found to be superior to Vertporfin (Photodynamic therapy) in predominantly classic neovascular age related macular degeneration with low rates of serious ocular adverse effects.
Triamcinolone is a slow releasing steroid preparation which helps in reducing the swelling associated with the disease and also has some anti-angiogenic action. The risk of increased intraocular pressure is its major disadvantage. Since it is a suspension it is visible as a floater in the upper field of vision for a few weeks after injection.
Intravitreal injections are given with aseptic precautions in an operation theatre. The eye is numbed with anesthetic drops and then the injection is given. The procedure is relatively atraumatic but carries a small risk of post injection infection, raised or low intraocular pressure, cataract formation, vitreous hemorrhage, retinal detachment. Systemically anti-VEGF agents are to be used with caution in patients with a recent history of cardiac ailment, uncontrolled hypertension and severe proteinuria.
Combination Therapy
Treatment of wet ARMD with Photodynamic Therapy (PDT) alone has very limited chances of visual improvement while anti-VEGF agents have the problem associated with repeated injections. Combination therapy of PDT with anti-VEGF agents or Triamcinolone makes the treatment more finite, with the advantage of improvement in visual acuity in some cases and reduced requirement for repeated injections
Transpupillary Thermotherapy (TTT)
In TTT, a large spot of diode laser (810 nm) with relatively low energy is applied to the area of new vessels. The treatment is non specific and there is concomitant damage to normal retinal tissue though less then in conventional laser photocoagulation.

Surgical Treatment
The following surgical procedures have been tried but with limited benefit:
Excision of Subfoveal CNVM R11; The technique for this has been fairly well perfected but visual recovery is limited by the fact that normal retinal pigment epithelial cells are also removed in the process.
Macular Translocation R11; In this procedure the retina is detached to be able to shift the fovea away from the subfoveal choroidal neovascular membrane. Thereafter the membrane is lasered without damaging the fovea. Drawbacks of this procedure are a high complication rate, inadequate shift of macula, formation of retinal folds and double vision.
Treatment Of Dry Age-Related Macular Degeneration
There is no definite treatment for the dry form but the AREDS (Age-related Eye Disease Study) found that a specific high dose formation of antioxidants and zinc significantly reduces the risk of advanced AMD and its associated vision loss. Regular Amsler grid monitoring to detect conversion of dry form to wet form is important. Smokers should ensure that the formulation they take does not contain Beta-Carotene as that may increase their risk of developing lung cancer.
Yearly complete eye check up
Regular Amsler monitoring once patient is diagnosed to have AMD.
Anti-oxidants to decrease progression of AMD.
Healthy diet rich in green leafy vegetables and fish.
Avoid smoking.
Maintain normal BP
Exercise and avoid obesity.
If you have lost sight from AMD do not be afraid to use your eyes for reading, watching TV.
Research
Scientists are studying the possibility of transplanting healthy cells into a diseased retina, and are evaluating families with a history of AMD to understand the genetic and hereditary factors that may cause the disease. They are also looking at certain anti-inflammatory treatments for the wet form of AMD.
This research should provide in the future, better ways to detect, treat and prevent vision loss in patient with AMD.
Vascular Occlusions
VASCULAR OCCLUSIONS
Occlusions of the retinal vascular system is the second most common retinal vascular disorder after diabetic retinopathy. They occur due to a blockage of the blood vessels which serve the retina.
SYMPTOMS
Painless loss of vision
Diagnosis is generally clinical
They can be of 2 Types
Venous occlusions
Arterial occlusions
Venous Occlusions are the more common of the two and has a better prognosis. The drop in vision in this disorder is generally due to thickening of the central part of the retina called the macula which is the area for fine vision
OCT is a useful non invasive diagnostic modality for diagnosing edema or swelling due to vascular occlusions. Fluorescein Angioigraphy is also performed to get to know about blood supply and to determine any risk of future bleeds in these eyes.
Recently intravitreal injections of anti VEGF agents and steroid injections/implants have shown good results in treating macular edema associated with venous occlusions. These may need to be repaeted frequently depending on the patients response to therapy.
Arterial occlusions are less common and are often associated with sever permanent vision loss.
Systemic factors like hypertension, cardiac history, high cholesterol and Diabetes are known to be associated with vascular occlusions. Your ophthalmologist may refer you to a physician or cardiologist in such cases.
Retinal Detachment
Retinal detachment is the separation of the retina from the underlying choroid. This results in a profound loss of vision and requires major surgery to re-attach it.
RETINAL DETACHMENT AND RETINAL TEARS
Retinal detachment and related vitreous problems affect one out of every 10,000 people each year. It is a sight threatening eye problem that may occur at any age although it usually occurs in middle-aged or older individuals. Surgery is often beneficial, and if done in time, can restore good vision. At Saraswati Nethralaya, we have a dedicated team of Vitreo-Retinal specialists committed to provide you with the best possible care to protect your vision.
What causes retinal detachment?
Most retinal detachments are caused by the presence of one or more tears or holes in the retina. Normal aging can sometimes cause the retina to thin and develop holes, but more often these are caused by shrinkage of the vitreous body (posterior vitreous detachment).
The vitreous is firmly attached to the retina in several places around the back wall of the eye. As the vitreous shrinks with aging, it may pull a piece of retina with it, leaving a tear or hole in the retina. Fluid from the vitreous body then passes through the retinal tear detaching the retina from its normal position (retinal detachment).
Posterior vitreous detachment (vitreous separation from the retina) is a natural process of aging and usually does not lead to any damage of the retina. It is however more common and occurs earlier in people who
- Are abnormally nearsighted (high myopia);
- Have undergone cataract operations (aphakics);
- Have had YAG laser surgery of the eye;
- Have had inflammation inside the eye
It should be noted that there are some retinal detachments that are caused by other diseases of the eye such as tumors, severe inflammations, or complications of diabetes. These so-called secondary detachments do not have tears or holes in the retina and treatment of the disease that caused the retinal detachment is the only treatment that may allow the retina to return to its normal position.
How is a person to know of the presence of retinal weakness, holes or tears?
In some patients the formation of a retinal tear is preceded by flashes of light, which are indicative of pull (traction) on the retina. In others, the tear may break a small blood vessel in its path causing a small hemorrhage (bleeding), with blurring of vision and floaters

However in the majority, retinal holes are completely asymptomatic, as they usually occur in the periphery of the retina and not in the visually important central part. They therefore do not cause any visual problem at all, unless they have led on to a retinal detachment. At this stage, profound loss of vision or field occurs.
It should also be noted that floaters are very commonly seen by people who have no eye disease. They are seen as small specks, circles, lines, clouds or cobwebs moving in one's field of vision. They are actually tiny clumps of gel or cells inside the vitreous and cause no harm.
Routine examination by binocular indirect ophthalmoscopy by a person proficient in this method is the only way holes or tears may be detected before they can cause retinal detachment.
What can be done about floaters?
Floaters can get in the way of clear vision, which may be annoying when you are trying to read. You can try moving your eyes; looking up and then looking down to move the floaters out of the way. While some floaters may remain in your vision, many of them will fade over time and become less bothersome. However you should visit your ophthalmologist if you suddenly notice new floaters because you need to know if your retina is torn.
What causes flashing lights?
When the vitreous gel rubs or pulls on the retina, you may see flashing lights or lightning streaks. If you notice the sudden appearance of light flashes, you should visit your ophthalmologist immediately to see if your retina has been torn.
Who runs a greater risk of developing such a problem?
People more prone to developing retinal degeneration, holes and tears, and subsequently retinal detachment are myopes (near sighted persons), aphakics (people who have undergone cataract surgery), those with a family history of retinal detachment and people with symptoms like light flashes and onset of a large number of floaters.
These groups of patients must undergo regular and thorough retinal examination by indirect ophthalmoscopy.
How can retinal detachment be prevented?
A careful examination of your retina by binocular indirect ophthalmoscopy as mentioned above will be done. For this procedure, your pupils will be dilated with eye drops. During this painless examination, your ophthalmologist will carefully observe your retina and vitreous and look for holes and weak areas. At this stage (i.e. retinal detachment has not yet occurred), they can easily be closed or sealed by producing minute scars in the retina around them, which weld the retina to the choroid and prevent fluid from seeping through the hole. These scars can be produced by the heat of a strong light source (laser photocoagulation), or by controlled freezing (cryotherapy). Which of these two modalities is chosen, depends on the location of the hole and the presence or absence of cataract and vitreous hemorrhage, and the retinal surgeon decides individually for each case after a thorough examination. Both cryotherapy and photocoagulation are usually carried out as an outpatient procedure. As the treatment is from the surface of the eye, no invasive surgery is involved.
Symptoms of retinal detachment
Some retinal detachments may begin without noticeable floaters or light flashes. In those instances, patients may notice a wavy or watery quality in their overall vision or the appearance of a dark shadow in some part of their side vision. Further development of the retinal detachment will blur central vision and create significant loss of sight in the eye unless the detachment is repaired.
A few detachments may occur suddenly and the patient may experience a total loss of vision in one eye. Similar rapid loss of vision may also be caused by bleeding into the vitreous when the retina is torn.
Detection & diagnosis
A detached retina cannot be viewed from the outside of the eye. Therefore, if the above symptoms are noticed, an ophthalmologist should be visited as soon as possible. Again, binocular indirect ophthalmoscopy through dilated pupils is essential to thoroughly examine the retina. Other special instruments including contact lenses, slit lamp and ultrasound may also be used.
Treating retinal detachment:
If the retina has become detached and the detachment is too large for laser treatment or cryotherapy alone, surgery is necessary to re-attach the retina. Without some type of retinal re-attachment surgery, vision will almost always be lost.
Scleral Buckling
The traditional surgery for retinal detachment is scleral buckling and is performed in the operation room under local or general anesthesia. In this process, after cryotherapy is done to seal the retinal tears, a piece of silicone plastic is sewn onto the outside wall of the eye (sclera) over the site of the tear. This pushes (buckles) the sclera in toward the retinal tear and holds the retina against the sclera until scarring from the cryotherapy seals the tear. This procedure is usually combined with placement of an encircling silicone band around the circumference of the eye to lessen the pulling of the vitreous on the retina. The surgeon may also drain fluid from underneath the retina and place a gas or air bubble into the vitreous cavity. These buckles and bands are left permanently and are not visible from outside. Success rates for re-attaching the retina with scleral buckling are approximately 90-95%.
Pneumo-retinopexy
This is another type of surgery for re-attaching the retina. Instead of placing a buckle after cryotherapy, the surgeon injects a gas bubble inside the vitreous cavity of the eye. The patient is instructed to keep his or her head in a specific position so that the gas bubble seals the retina tear by its surface tension effect. Circulation of fluid through the tear stops and the retina is re-attached.

Vitrectomy
Vitreous surgery is now routinely undertaken for primary detachments especially in patients who have already had cataract surgery done previously. It is especially useful in cases when the tears are very large or placed very far back (posteriorly) on the retina, when there is a macular hole causing detachment, or if there is blood in the vitreous blocking a clear view of the retina. Success rates for these cases are much better with vitrectomy than with scleral buckling.
Occasionally, retinal detachment is so complicated and severe that it cannot be treated with either standard scleral buckling surgery or pneumatic retinopexy. Moreover scleral-buckling surgery fails approximately 5% to 10% of the time because excessive scar tissue grows on the surface of the retina. This scar tissue is very bad for the eye. It pulls on the retina, causing it to re-detach. Retinal re-detachment usually occurs four to eight weeks after the initial surgery. The vitreous pulls on the retina, detaching it from the back wall of the eye. The scar tissue also puckers the retina into stiff folds, like wrinkled aluminum foil. This condition is called proliferative vitreo-retinopathy (PVR).
The only way to unfold and re-attach the retina is to cut away the vitreous and remove the scar tissue with vitrectomy surgery and then re-attach the retina. The surgeon uses a fibre-optic light to illuminate the inside of the eye and a variety of instruments (scissors, forceps and laser probes). The vitreous gel is removed as well as abnormal scar tissue, and replaced with fluid or air. Sometimes the natural lens or a previously existing intraocular lens (IOL) may have to be removed if the case is complicated. The holes and tears are sealed with laser, and fluid under the retina is drained. At times, vitrectomy is combined with placement of a scleral buckle. Often air, gas or silicone oil is placed in the vitreous cavity to hold the retina in place. If silicone oil has been used, it has to be removed at a later date as a separate surgical procedure.
Removing the vitreous and especially the scar tissue from the surface of the retina is a delicate process that requires the surgeon to lift and peel strands of scar tissue away from the retina. The surgery may take many hours in severe cases.
If the retina is successfully re-attached, the eye will recover some sight, and blindness will have been prevented. However, the degree of vision that finally returns up to six months after successful surgery depends upon a number of factors. Unfortunately, success in re-attaching the retina (anatomic success) does not always translate into marked visual improvement (functional success). This is because of permanent damage to fine vision cells of the macula. In general, there is less visual return when the retina has been detached for a long duration, or there is a fibrous growth on the surface of the retina. It should be clearly understood that often the purpose of surgery for PVR is to give the patient an eye that would have some supporting vision and could serve as a spare tyre, if the other eye ever loses vision entirely.
Microincision Vitreous Surgery (MIVS) with smaller instrument size is the latest revolution in Vitreous surgery. The finer instrumentation allows one to perform technically complex steps with greater safety. This translates into better visual outcomes and faster healing and recovery for our patient. This technique allows us to safely operate closer to the retina for peeling of fine membranes from the surface of the retina.
What are the complications of surgery?
Even though the surgery for retinal detachment is generally successful, certain complications can occur. They include drooping of the upper lid and double vision, which are temporary. Serious complications include infection, bleeding severe enough to interfere with vision, glaucoma and cataract formation. However, these complications are very infrequent. Retinal re-detachment is the most commonly occurring problem. If this occurs, your surgeon will discuss the chance that a re-operation will successfully re-attach the retina. It is important for the patient to know that surgery may fail due to complications, or simply due to the progressive nature of the retinal disease.