Medical Ophthalmology
At Saraswati Nethralaya, we have a dedicated team of eye specialists committed to provide you with the best possible care, to protect your vision. For a routine but comprehensive eye check up, make an appointment with one of our consultants. Every patient at Saraswati Nethralaya is routinely tested for visual acuity (testing of the eyesight) and eye pressure is measured to screen for glaucoma.
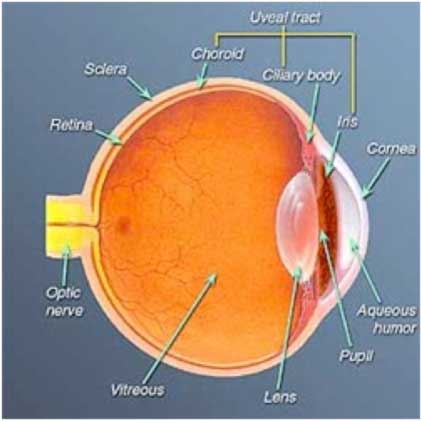
NORMAL STRUCTURE OF THE EYE
The eyeball can be divided into three coats or tunics. The outer white coat, or sclera, forms a dense, fibrous outer covering. In the front part of the eye the sclera becomes continuous with the cornea, the transparent structure through which we see. The innermost lining of the eyeball, is a thin layer known as the retina (image-gathering tissue in the back of the eye much like the film in a camera), which contains the nerve endings whose function it is to send visual impulses to the brain. These nerve fibers form the optic nerve, which exits through an opening in the back part of the sclera. The eyeball cavity is filled with a jelly-like substance called the vitreous.
The layer between the sclera and the retina is the uvea or uveal tract, the pigmented middle coat that is made up of three parts:
1. The iris is the colored portion in the front part of the eye; it has a circular opening in the middle, the pupil, which dilates and contracts in response to light.
2. The ciliary body is the middle part of the uveal tract, which produces the fluid inside the eye (aqueous humor). It comprises of very fine muscles and ligaments that attach to the capsule of the lens of the eye and help in varying the focus of the eye. The lens is a transparent semisolid body enclosed in a transparent capsule. The contraction and relaxation of the ciliary muscle are what enable the lens to modify its shape, allowing the eye to focus as it looks from one object to another.
3. The choroid is the back part of the uveal tract and lies just outside the retina. The blood vessels contained within the choroid provide vital nourishment for the eye.
ROUTINE EYE TESTING:
Children should undergo routine eye examinations once a year, especially if he or she complains of symptoms such as headache, tired eyes or inability to see the blackboard clearly.
Glasses for children should be made of shatterproof plastic or case hardened material. Children should wear their prescribed glasses constantly.
Any pre-school child with a squint (eyes appearing to be crossed) needs to be urgently examined by an ophthalmologist.
Adults should have their eyes tested completely every one to three years.
PREVENT EYE INJURIES:
Make sure all spray nozzles are directed away from you.
Read instructions carefully before using cleaning fluids, detergents, ammonia or harsh chemicals. Wash your hands thoroughly after use.
Pay attention to your childR17;s age and responsibility level when you buy toys and games. Avoid projectile toys such as darts, pellet guns, etc., which can hit the eye from a distance.
Supervise children when they are playing with toys or games that can be dangerous.
Teach children the correct way to handle items such as scissors and pencils.
Never allow children to ignite fireworks.
Do not stand near others when lighting fireworks.
HOW TO USE EYE DROPS:
First, wash and dry your hands thoroughly.
Check you have the correct bottle, and make sure you know which eye the drops are to go in.
Stand in front of the mirror, sit in a chair, or lie down, which ever is best for you.
Take the top off the bottle, lean your head back, and look up at the ceiling.
Pull down your lower eyelid and squeeze a drop into you eye, taking care not to touch the eye with the tip of the bottle.
Close your eyes for 2 minutes, and wipe gently with a clean tissue, if necessary.
Put the top on firmly back on the bottle and put in a safe place.
Finally, wash your hands again.
Remember:
DO NOT share your drops with anyone else.
Bottles of eye drops should only be used for four weeks after opening.
It may help to write on the label, the date you open the bottle.
It may also help to identify different drops by sticking a colored label on the bottle.
Your drops can be kept in the fridge but do not freeze them.
You can get more drops on prescription of your eye doctor.
Important: Use drops in the frequency and for the duration recommended by your doctor.

WHAT IS COMPUTER VISION SYNDROME?
Computer Vision Syndrome (CVS), a relatively new condition, is the complex of eye and vision-related problems associated with computer use affecting millions of people. The primary symptoms are eyestrain, blurred vision, dry and irritated eyes, tired eyes, and headaches. Neck and backaches can also be related to the way that we use our eyes at the computer.
• This happens because staring at a computer screen causes a significant reduction of the normal blink rate. Hence washing of the corneal surface of the accumulated dust, debris and tear waste products is delayed; instead they have a longer contact time with the cornea producing ocular surfacing problems and eye fatigue. The following steps can help alleviate your symptoms:
To ensure comfort while working on the computer:
Lower your computer screen so that the center of the screen is 4-8 inches below your eyes.
Ensure correct posture, adequate room lighting and convenient placement of the mouse and keyboard.
Use an anti-reflection filter over your monitor to avoid glare and eyestrain.
If you are seated in a draft or near an air vent, try to eliminate the flow of air past your eyes. Low humidity or fumes aggravate a dry eye condition. If you have these conditions in your work place, fix them if possible.
Concentrate on blinking whenever you begin to sense symptoms of dry or irritated eyes.
Every once in a while (especially when you sense the symptoms) close your eyes and roll them behind your closed eyelids.
Take a short break of a few minutes from your work, every half an hour.
Use artificial tears to re-wet and lubricate your eyes as recommended by your doctor.
You should seek professional eye care if symptoms persist. Many computer users need a pair of glasses for their computer work that is different from the glasses they use for their other common visual needs. They either have a different prescription or a different lens design from their usual glasses. A thorough check up by an ophthalmologist is essential to identify and treat the factors contributing to the problem.
YOU COULD BE HAVING CATARACT IF YOU HAVE:
Cloudy, fuzzy, fogging, or filmy vision.
Changes in the way you see colors.
Problems driving at night because headlights seem too bright
Problems with glare from lamps or the sun.
Frequent changes in your eyeglass prescription.
Double vision or multiple images.
Better near vision for a while only in farsighted people.
These symptoms also can be signs of other eye problems. See your eye doctor to find out what you have and how it can be treated.
GLAUCOMA:
If you are 40 years of age, or have a family history of glaucoma you should have your eyes tested regularly. See your eye doctor to arrange a test.
If you have glaucoma, regular eye tests for pressure and the visual field, and taking your treatment properly can prevent blindness.
DIABETES AND EYE CARE:
an eye with marked changes of Diabetic Retinopathy can have good vision and be totally free of symptoms.
Hence it is important for all diabetics to undergo regular eye check-up including retinal examination through dilated pupils especially for people who have been diabetic for a number of years.
It is also true that diabetes is often detected in a person, when some changes of retinopathy are seen on routine examination of the eye.
YOU COULD BE HAVING RETINAL TEARS & DETACHMENT IF YOU HAVE:
If you notice the sudden appearance of light flashes, or if you suddenly notice a large number of floaters, you should visit your ophthalmologist immediately to see if your retina has been torn.
Myopes (near sighted persons), aphakics (people who have undergone cataract surgery), those with a family history of retinal detachment are more prone to developing retinal degeneration, holes and tears, and subsequently retinal detachment. These groups of patients must undergo regular and thorough retinal examination by indirect ophthalmoscopy.